America’s Healthcare Crisis–Part II–What Do We Get for $$$ ?
IV. What Do We Get for All That Money?
According to the Kaiser Foundation:[1]
The number of prescriptions filled in the US increased 72% from 1997 to 2007.![]()
US prescriptions rose to 3.9 billion in 2009 and sales reached $300.3 billion.
Pharma profits have been in the double digits since 1995—far surpassing Fortune 500 companies.
In 2009, pharmaceutical companies raked in the highest profit ever, 19.8%.
However, those corporate profits were not earned by producing therapeutically beneficial medicines that cured disease or improved Americans’ health. Indeed, Americans would be shocked to learn that the staggering expenditure for prescription drugs—in most cases—did not get them treatments that improved their health. Analysis of FDA drug approvals demonstrates that only 1 in 10 new drugs offers clinical benefits for patients compared to existing much cheaper drugs. In his book, The Risks of Prescription Drugs (2010),[2] Dr. Donald Light analyzed the data for new FDA-approved drugs over the last twenty years and found that only 2%-3% represent a real clinical breakthrough and another 11% offer some advantage over existing drugs. His findings confirm numerous independent reviews—including industry assessments (1996)[3] that found only 11% of new drugs (1974-1994) were therapeutically and pharmacologically innovative.
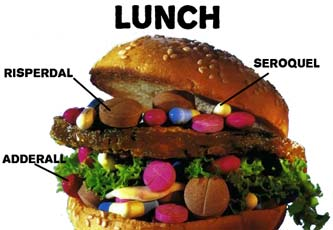
Polypharmacy: the prescribing of multiple drugs in untested “cocktail” combinations of antipsychotics and SSRI antidepressants has become the “norm and practice” in psychiatry. Psychiatrists from Johns Hopkins and Columbia University examined “National Trends in Psychotropic Medication Polypharmacy in Office-Based Psychiatry,”(2010) [4] and found that 60% of patients seeing a psychiatrist received at least two prescriptions for psychotropic drugs, and 33% received three or more prescriptions. This was a median 40% increase between 1996 and 2006. Prescriptions were for two or more antidepressants, antipsychotics, sedative-hypnotics, and antidepressant-antipsychotic combinations.
“While some of these combinations are supported by clinical trials, many are of unproven efficacy. These trends put patients at increased risk of drug-drug interactions… there is growing evidence regarding the increased adverse effects associated with such combinations.”
Polypharmacy is an example of a clinically unsupportable current practice that has increased industry’s profits exponentially by exposing millions of patients to potential serious harm. Indeed, even Dr. Steven Stahl[5] called polypharmacy a “dirty little secret” that “seems to be something everybody does and nobody admits.” He acknowledged that:
“Using 2 antipsychotics at the same time is perhaps the most expensive, most widely practiced, yet least evidence-based therapeutic option in psychiatry today.”
Widespread, indiscriminate prescribing of the newest psychotropic drugs—in particular, SSRI antidepressants and antipsychotics—have made them industry’s blockbuster profit makers—despite a huge body of evidence demonstrating that they have caused profound harm–[6] including, birth defects, triggering suicide, and precipitating severe, debilitating, life-shortening irreversible diseases such as diabetes and cardiovascular disease. If judged by the “First, do no harm” principle, such a practice would constitute malpractice. The vast majority of prescriptions for multiple psychotropic drugs are paid for by taxpayers through Medicaid and Medicare. The author of Anatomy of an Epidemic[7] argues that the skyrocketing increase in the number of Americans on government disability due to mental illness—from 1.25 million in 1987, to more than 4 million in 2011—is a consequence of the high use of multiple psychotropic drugs.
The preventable harm and waste in America’s healthcare system is in large part the consequence of a medical provider system—that includes hospitals, medical specialty societies, and the American Medical Association—who are aligned with healthcare industries—insurance, pharmaceutical and medical device manufacturers. All of these interlocking self-interest groups are major contributors to Congressional and presidential election campaigns—ensuring that their interests are reflected in public health policies.
V. A preventable epidemic of injury and death is caused by FDA-licensed prescription drugs.[8]
“With an estimated 2 to 4 million serious injuries each year, drug therapy stands as one of the most significant perils to health resulting from human activity.”[9]
 An analysis in JAMA (2002)[10] identified 548 prescription drugs approved between 1975 and 1999.
An analysis in JAMA (2002)[10] identified 548 prescription drugs approved between 1975 and 1999.
The authors found that life-threatening adverse drug effects were identified long after the drugs had been
marketed: 56 new drugs (10.2%) subsequently acquired Black Box warnings or were withdrawn;
45 new drugs (8.2%) acquired more than one Black Box warning. The authors reported that the probability
that a new drug will produce adverse effects so severe as to acquire a Black Box warning or being withdrawn
from the market is 20%. Their conclusion: “Adverse drug reactions are believed to be a leading cause of death…
The safety of new agents cannot be known with certainty until a drug has been on the market for many years.”
The Institute of Medicine reported (2007)[11] that each year, 1.5 million Americans are injured or killed by preventable prescription medication errors at an estimated cost of $3.5 billion for additional medical treatment. The report noted that 215 prescription drugs and 71 over-the-counter drugs were recalled in 2004 due to either manufacturing problems or adverse drug reactions.
An NIH Pharmacoepidemiology Drug Safety report (2010)[12] analyzed outpatient data over an 11- year period (1995-2005). The authors note that “estimates of the proportion of outpatients who experience an adverse drug effect (ADE), and seek medical attention have ranged from 16% to 48%.” They found that 15.5 people per 1,000 sought medical attention for ADEs: among the elderly, the rate jettisoned to 47.0 ADE visits per 1,000.
The authors estimated that more than 4.3 million Americans sought medical care for adverse drug events annually—of these, 791,000 sought hospital emergency care. The report fails to disclose the number of deaths. The authors note, “Strikingly the proportion of patients taking 5 or more drugs doubled between 1995 and 2005.”
A QuarterWatch (2007)26 analysis of adverse drug reactions (ADRs) reported to FDA’s MedWatch between 1998 and 2005, found that ADRs nearly tripled from 156,000 to 460,000. The reports constitute only 1% to 10% of actual toxic drug side effects because doctors who prescribe the drugs are loath to attribute deaths and severe adverse effects to medicines they prescribe.
A recent QuarterWatch analysis (2012) estimated that prescription drugs were linked to 45 million to 50 million ADRs annually: 2.5 million to 4 million were serious, disabling or fatal.26
FDA’s Contribution to the epidemic: The FDA accommodated industry by lowering the approval standard for efficacy while maintaining an irrational safety standard: FDA accepts trial results that only meet surrogate endpoints instead of clinical outcomes, and approves drugs that only demonstrated “non-inferiority”[13] to a comparator drug—which effectively requires a new drug not to be “unacceptably worse” than an existing drug.
FDA’s irrational safety standard does not recognize a potentially lethal risk unless it can be proven with 95% certainty. This Daredevil public health policy gambles with lives by adhering to a Russian roulette safety standard. This has resulted in the approval of medicines that were less effective and posed higher risks than existing ones.
Since 1992, there were 28 drugs that were subsequently withdrawn for safety reasons after causing catastrophic harm to millions of people.
Among these were Propulsid, Redux, Baycol, Trovan, Rezulin, Vioxx, Bextra, Tysbari, Avandia, Tequin, and Xigris…
There were 17 drugs withdrawn that had been approved prior to 1992. ![]()
See, List of drugs recalled for safety issues from 1980-2011.
VI. Big Pharma’s business model: manufactured myths, propaganda and a hidden agenda.
The Prescription Drug User Fee Act (PDUFA 1992)[14] was enacted to eliminate perceived obstacles to bringing innovative drugs to market by reducing the time for review and approval. But PDUFA’s user fees effectively undermined FDA’s independence and its ability to carry out its mission of protecting the public health from unsafe and ineffective medical products.
Almost half of FDA’s budget is dependent on industry user fees. PDUFA exposed the FDA to undue industry influence, allowing pharmaceutical companies ready access to FDA officials behind closed doors—thereby ensuring that industry’s interests would take precedence over public safety. The FDA has accommodated industry by accelerating the approval process for new drugs and medical devices that have not been adequately tested prior to licensure.
The result is measurable in extraordinary profits for pharmaceutical companies and human casualties.
How ironic then, that twenty years after PDUFA, the pharmaceutical industry has once again promulgated the idea that onerous regulatory obstacles have resulted in what industry calls, an “innovation crisis.” Two current articles challenge the pharmaceutical industry’s fabricated claims that “innovative” medicines are not being produced because of regulatory burdens. The specious claim has led the FDA to further loosen its safety standards for approval of new drugs—even as their undisclosed, severe adverse effects have led to millions of preventable fatalities and disabling injuries.
Dr. Donald Light and Dr. Joel Lexschin in a recent article in the BMJ, (2012) [15] debunk several Pharma promulgated myths. First, they show how the pharmaceutical industry generated a barrage of articles and press reports promulgating a myth about a so called “innovation crisis” due to onerous regulatory obstacles. A myth that is belied by several analyses of the data—including an analysis by a Pfizer team (2005) that concluded, the claimed innovation crisis “bears no relationship to the true innovation rates of the pharmaceutical industry.” FDA’s accelerated approval process refutes Pharma’s claims that regulatory obstacles prevent innovative drugs from reaching the public.
From 2000 to 2010, the FDA awarded priority review to 44% of new drugs approved —despite lack of therapeutic value.
Second, they refute industry’s inflated claims about the high cost of research and development in bringing a new drug to market. Industry misrepresents the research and development (R & D) cost as $1.3 billion—half of which includes estimated unearned presumed profits from investments, and by including the cost borne by taxpayers. Those inflated estimates do not factor in the six-fold increase in revenues between 1995 and 2010. Stripped of some of the inflated illegitimate cost estimates, the authors estimate the cost of R & D for bringing a new drug to market at between $60 million and $90 million.
“Both claims serve to justify greater government support and protections from generic competition, such as longer data exclusivity and more taxpayer subsidies.”
The real health crisis is the miniscule number of clinically beneficial safe new drugs:
“How have we reached a situation where so much appears to be spent on research and development, yet only about 1 in 10 newly approved medicines substantially benefits patients? The low bars of being better than placebo, using surrogate endpoints instead of hard clinical outcomes, or being non-inferior to a comparator, allow approval of medicines that may even be less effective or less safe than existing ones.” [15]
Thomas Moore and Dr. Curt Furberg demonstrate in am artoc;e om JAMA (2012)[16] how safety was sacrificed when the Obama Administration and the FDA embarked on the so-called “biomedical innovation” initiative.
“Although enabling new drugs with a favorable benefit-to-harm balance to become available to patients more rapidly is a laudable goal, the underlying question is what public health risks are taken when drugs are approved for widespread use while important safety questions remain unanswered.”
“In its fiscal year 2011 summary, the FDA classified every new molecular entity as “innovative” and reported using 1 or more expedited approval programs for 16 of the 35 new drugs (46%). All 16 of these drugs received Priority Review, which provide shortened review times for drugs that may offer a therapeutic advance; 13 drugs were also designed for the Fast Track program which allows reviews to begin before clinical studies are complete for drugs that may fill serious unmet medical needs, and 3 drugs received Accelerated Approval, a program that relies on preliminary but not definitive evidence of benefit.”
The FDA has been serving as industry’s handmaiden, expediting approval of drugs that offer no potential therapeutic benefit. The FDA has even disregarded the safety concerns of FDA scientists who detected potential serious risks, insisting that the risks have not been proven with 95% certainty.
FDA’s priority has been directed at facilitating the marketing of patent protected drugs which companies misrepresent, widely promoting them as “breakthrough” innovative medicines which are priced much higher than existing drugs—as reflected in the exceedingly high expenditure for prescription drugs that Americans are saddled with.
The real cause of Pharma’s innovation crisis is a dubious business model and US patent policy.
The paradox—and the key to Big Pharma’s business model –is that the most profitable “blockbuster” drugs are the least innovative, offering marginal, if any, clinical benefits. Their market success—even as they’ve been shown to cause serious harm—relies entirely on costly marketing campaigns.
Their short-term business success begets an array of “me too” drugs by competing companies, as well as reformulations of the same drug—an unethical strategy extending patent protection in order to prevent the marketing of much cheaper generic versions. This counterproductive tactic is facilitated by US patent policy.
Influential pharmaceutical industry rebels are for calling for “transformational change.” In articles published in Science Transitional Medicine, [17] two highly regarded critics of the pharmaceutical industry’s current R & D model, Bernard Munos and Dr. William Chin, both had held senior executive positions at Eli Lilly, argue that:
1. “The sharing of knowledge has been one of the main forces driving science and innovation. Yet in recent decades, a proprietary culture, which wrongly posits that all intellectual property must be restricted, has spread across the pharmaceutical industry and threatens to stall the engine that has given us so many valuable treatments.
2. “Pharmaceutical companies, together with universities and government agencies, stand to gain much from reversing that trend and engaging in widespread collaboration early in the research process to expand foundational knowledge and create a shared infrastructure to tap it.”
3. The business model that works for portfolio fund managers is the wrong model for encouraging scientific innovation.
“Over the past 20 years, pharmaceutical companies have implemented conservative management practices to improve the predictability of therapeutics discovery and success rates of drug candidates. This approach has often yielded compounds that are only marginally better than existing therapies, yet require larger, longer, and more complex trials. To fund them, companies have shifted resources away from drug discovery to late clinical development; this has hurt innovation and amplified the crisis brought by the expiration of patents on many best-selling drugs.”
In interviews in Forbes (2011)[18] and at Duke University’s Kenan Institute for Ethics (2012),[19] and in comments that he posted on the blog, Pharmalot (2012),[20]
Mr. Munos criticized Pharma’s corporate culture, identifying four core values—ethics, risk taking, real innovation and patient needs—the pharmaceutical industry abandoned those core values during the last 10-15 years.
Ed Silverman’s post (Pharmalot) about reformulations elicited the following comments from Mr. Munos:
“These are the kind of practices that bring discredit upon the industry. They trample the values that have made it great such as focusing on breakthrough therapies, and putting patients at the center of what we do. Is it legal? Apparently yes. Is it ethical? No, not by any standard.”
“Drug company leaders should keep in mind that this is no ordinary industry. It has a covenant with society. It gets IP [intellectual property] protection, which is essentially a license to print money, but in exchange, society expects novel therapies. If industry fails to live up to their part of the bargain, perhaps it is appropriate for society to revisit its end as well. And it could do so by scaling down the IP protection that industry has misused. Abbott has only registered 2 drugs with FDA in the last 10 years, the lowest number among big pharma.”
“…ethical and legal violations by pharma companies have become so common that they overwhelm the litigation abilities of states, even large states such as Texas. When I joined the pharma industry in 1980, it was routinely called “the ethical pharmaceutical industry”. Today, hardly anyone dares say this again… over the last 20 years, pharma companies have been fined over $20 billion for misbehavior, most of that in the last 5 years, becoming by that standard the second most tarnished industry after tobacco (but ahead of arm-dealers). This is a problem, and somebody has to own it. And when it comes to ethics, the responsibility starts at the very top, because CEOs set the culture for their companies.”
A continuing cascade of civil and criminal lawsuits against pharmaceutical companies provides hard evidence of serious safety hazards posed by FDA approved prescription drugs. They also substantiate the charge that pharmaceutical companies operate as “criminal enterprises.”
The documents reveal that companies engage in fraud and deceptive marketing tactics to promote drugs they know to cause harm. To bolster sales, companies deceive doctors and the public by making fraudulent claims about benefits not supported by evidence, while concealing life-threatening risks of harm.
As Senator Bernard Sanders put it, “a culture of fraud permeates the pharmaceutical industry. Over the past decade, virtually all the major private pharmaceutical companies were involved in significant health care fraud.”[21]
See, Pharma Criminal Rap Sheet a sample of major criminal/ civil Settlements. See also, update.[22]
See, List of Prescription Drugs Recalled for Safety Issues from US Market:
See also, www.RxISK.org a new interactive website that seeks consumer input about adverse drug effects.
Dr. Marcia Angel, [23] a thoughtful critic has been writing extensively about how drug companies exploited the Bayh-Dole Act (1980) to gain nearly limitless influence over medical research, education and practice guidelines. The law was enacted to spearhead the rapid transfer of innovative technology to industry by opening the way for public-private partnerships between academia and industry by encouraging universities and individual academics to patent research discoveries made through government funded grants, and to license those patents to companies for production and marketing. In exchange, the academics and universities are paid royalties.
But as Dr. Angel has been pointing out, the law ushered in major financial conflicts of interest, “dissolving the important differences between their missions [which] are becoming blurred. Medical research, education, and clinical practice have suffered as a result.”
Perhaps, just maybe, Dr. Starfield’s warning about “the harmful effects of health care interventions, and the likely possibility that they account for a substantial proportion of the excess deaths in the United States compared with other comparably industrialized nations,” is beginning to sink in about the imperatives for changing the focus of research and health policy.
A growing number of physicians and 5 major medical specialty associations acknowledge that medically unsupportable interventions pose serious risks of harm.[24]
In the absence of demonstrable clinical benefits, they recommend LESS diagnosing of presumed, unsubstantiated conditions, LESS medically unjustifiable testing, and LESS prescribing of invasive treatments and drugs.
A recent Op Ed by H. Gilbert Welch, MD , Professor of Medicine, Dartmouth, and author of the book, “Overdiagnosed: Making People Sick in the Pursuit of Health,”[25] states:
“Medical research is dominated by research on the new: new tests, new treatments, new disorders and new fads. But above all, it’s about new markets. We don’t need to find more things to spend money on; we need to figure out what’s being done now that is not working…we have to start directing more money toward evaluating standard practices.”
See, Medicine Hijacked AHRP compilation of 100 books by prominent physicians and knowledgeable independent healthcare analysts who confront the real healthcare crisis from varying aspects. The authors have come to the sobering conclusion that the current uncoordinated, duplicative, error-riddled system is unsustainable. Not only are commercially-driven medical practices—such as over prescribing of new, not better drugs, overuse of diagnostic radiology tests, and invasive interventions–bankrupting American taxpayers, the treatments are causing an epidemic of preventable, iatrogenic injury and death.
Vera Sharav
This is Part II of IV.
See, Part III: The Untouchable Third Rail in Healthcare—The Vaccine Controversy: Core Issues
Part IV: FDA, A Complicit Partner of Crimes and Corrupt Industry Practices
See also, Part I: America’s healthcare crisis is demonstrable ; America’s ranking has plummeted compared to the industrialized world; The third Leading cause of death is medical intervention; Commercially profitable, wasteful, inefficient and exceedingly harmful.
REFERENCES
[1] Kaiser Family Foundation. Prescription Drug Trends, 2008; Prescription Drug Trends, 2010; Profitability of pharmaceutical manufacturers, 1995-2009.
[2] Light D. The Risks of Prescription Drugs, Columbia University Press, 2010.
[3] See, Barral, P E. “20 Years of Pharmaceutical Research Results Throughout the World: 1975–94” Paris: Rhone-Poulenc Rorer Foundation, 1996. See also, “A Look Back at Pharmaceuticals in 2006: Aggressive Advertising Cannot Hide the Absence of Therapeutic Advances,”Prescrire International 16 (2007): 80–86.
[4] Mojtabai, R and Olfson, M. “National Trends in psychotropic Medication Polypharmacy in Office-Based Psychiatry,” Archives of General Psychiatry, 2010, vo. 67.
[5] Steven Stahl, MD, PhD is a prominent academic who trained in three medical specialties—neurology, internal medicine and psychiatry—with extensive consultancies with all the major pharmaceutical companies. Stahl, S. “Antipsychotic Polypharmacy Therapeutic Option or Dirty Little Secret?” J of Clinical Psychiatry, 2002. See also, Stahl, SM. Brainstorms. “Antipsychotic Polypharmacy: Squandering Precious Resources?” J Clin Psychiatry 2002; 63:93-94.
[6] See, Healy, D. Pharmageddon, U of California Press, 2011; Unexamined Drug Epidemic—the Elephant No One Wants; The Truth About Psychiatric Drugs; The Real Biederman Scandal;
[7] Whitaker, R. Anatomy of an Epidemic: Magic Bullets, Psychiatric Drugs, and the Astonishing Rise in Mental Illness in America, Crown Publishing, 2010.
[8] Lasser, KE, Allen,PD, Woolhandler,SJ, Himmelstein, DU, Wolfe, SM, Bor, DH, et al. “Timing of New Black Box Warnings and Withdrawals for Prescription Medications,” JAMA 287 (2002): 2215–20.
[9] Moore, M. Cohen, and C. Furberg, “Serious Adverse Drug Events Reported to the Food and Drug Administration, 1998–2005,” Archives of Internal Medicine, Sept, 2007, 167:16; and Moore TJ, Cohen MR, Furberg CD. (2012) QuarterWatch 2011 Q-4: Anticoagulants the Leading Reported Drug Risk in 2011.
[10] US Health Resources Services Administration. National Vaccine Injury Compensation Program. 2012.
[11] Institute of Medicine, Preventing Medication Errors: Quality Chasm Series (2007)
[12] Bourgeois, FT, Shannon, MW, Valim, C and Mandl, KD. Adverse Drug Events in the Outpatient Setting: An 11-Year National Analysis, Pharmacoepidemioly Drug Safety, 2010 September; 19(9): 901–910.
[13] Schumi, J and Wittes, JT. “Through the Looking Glass: Understanding Non-Inferiority,” Trials Journal, 2011:106.
[14] Prescription Drug User Fee Act (PDUFA) 1992. http://www.fda.gov/ForIndustry/UserFees/PrescriptionDrugUserFee/default.htm
[15] Light, D and Lexchin, J. Pharmaceutical research and development: what do we get for all that money? British Medical Journal (BMJ), 2012: 344
[16] Moore T and Furberg C, The Safety Risks of Innovation: The FDA’s Expedited Drug Development Pathway, JAMA, 2012.
[17] Bernard Munos, a 30-year Eli Lilly veteran, is now a consultant to pharmaceutical and biotech industries. Dr. William Chin moved from Harvard Medical School to senior V-P of research and clinical investigation at Lilly, is now Executive Dean for Research at Harvard. Munos, BH and Chin, WW. “A Call for Sharing: Adapting Pharmaceutical Research to New Realities,” Science Translational Medicine, 2009: Vol. 1, Issue 9; Munos, BH and Chin, WW. “How to Revive Breakthrough Innovation in the Pharmaceutical Industry,” Science Translational Medicine, June 2011;
[18] Herper, M. “Rallying Pharma’s Rebels, Forbes Magazine, August 8, 2011.
[19] “The Writing on the Wall,” Interview by Herzog, M. Kenan Institute for Ethics, June 12, 2012.
[20] Silverman, E. When Reformulations Are A really Bad Deal,” Phamalot, April 10, 2012
[21] Sen. Bernie Sanders. Crack Down on Pharmaceutical Fraud, May 23, 2012.
[22] Pharma Criminal Rap Sheet; On August 30, 2012 Janssen (J & J settled yet another lawsuit involving deceptive marketing of its antipsychotic drug, Risperdal. The settlement with 36 states is for $181 million: “This landmark settlement holds the companies accountable for practices that put patients in danger…” On September 10, 2012, J & J settled the first of dozens of individual case charging harm from Risperdal on the day the trial was to begin in Philadelphia.[22] Still pending is a federal case involving kickbacks to a nursing home—the penalty could exceed $2 billion.
[23] Angel, M. The Truth About Drug Companies, Random House, 2004; “Big Pharma, Bad Medicine,” Boston Review, May/June 2010.
[24] National Physicians Alliance. “Choosing Wisely,” The “Top 5” Lists in Primary Care Meeting the Responsibility of Professionalism,” Archives of Internal Medicine, 2011;171(15):1385-1390.
[25] Welch G. OpEd. “Testing Standard Medical Practices,” The New York Times, August 20, 2012.