In Medicine, the Power of No vs. Psychiatry’s Mass Overtreatment
New York Times columnist, David Leonhardt, applauds the new Medicare policy inaugurating comparative risk/ benefit analyses of medical treatments as a means of reducing healthcare costs–and also to reduce risks of serious side-effects from unnecessary treatments.
He notes the likely resistance by the public that has an ingrained instinct to "try-anything-and-everything," without regard for the evidence showing that unnecessary treatments are accompanied by serious adverse effects–including treatment-produced deaths.
He notes that "unnecessary care causes a lot of pain and even death."
The examples he cites as overused and medically unnecessary treatments:
Unnecessary and overused CT scans which will result in an estimated 15,000 deaths from radiation; unnecessary caesarean births; unnecessary prostate cancer treatments which leave men incontinent and / or impotent; the popularity of cardiac stenting–despite lack of evidence that they actually reduce heart attacks.
However, missing from the discussion entirely, is the current aggressive move by the American Psychiatric Association to redefine diagnoses by lowering–even eliminating–the clinical threshold of pathology.
The APA’s Expansionist DSM-V Strategy :
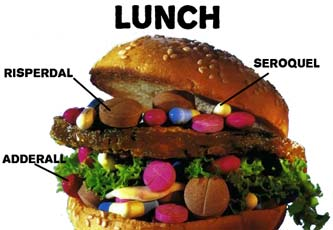
In lieu of clinical evidence of pathology, the APA proposes broadening the definition of diagnoses to its diagnostic / practice guide, the DSM-V, by lowering the threshold for existing diagnoses by adopting broad, nonspecific, "Risk Syndrome" diagnoses. This strategy will result in meteoric increase in healthy people being deemed mentally ill, for whom pharmacological interventions will be prescribed.
The APA DSM-V recommendations provide a rationale–though an unsubstantiated rationale–for EXPANDING the use of expensive, clinically insignificant, psychotropic drugs–thereby INCREASING the cost for mental health care.
The vague, nonspecific "diagnoses" defined by presumed risk include:
"Psychosis Risk Syndrome" which will pathologize mostly healthy children / adolescents who will be prescribed antipsychotics; "Mixed Anxiety Deppressive Disorder" will be a boon to antidepressant drug manufacturers; "Minor Neurocognitive Disorder" will pathologize everyone over age 50 as at risk for Alzheimer’s, no doubt exploding the market for drugs; "Binge Eating"; "Temper Dysfunctional Diorder" medicalizes temper tantrums;
As acknowledged by Dr. Allen Frances , Prof. Emeritus, former chairman of psychiatry, Duke University and the DSM-IV Task Force [1,2]:
"Among the most problematic suggestions for DSM-V, the proposal for a "Psychosis Risk Syndrome" stands out as the most ill–conceived and potentially harmful."
"The whole concept of early intervention rests on 3 fundamental pillars– being able to diagnose the right people and then providing them with a treatment that is effective and safe. "Psychosis Risk Syndrome" fails badly on all 3 counts:
1. It would misidentify many teenagers who are not really at risk for psychosis.
2. The treatment they would most often receive (atypical antipsychotic medication) has no proven efficacy, but. . .
3. It does have definite dangerous complications.
"It has been estimated that the false-positive rate would jump from about 70% in specialty clinics to about 90% in general practice. This means that as many as an astounding 9 in 10 individuals identified as "risk syndrome" would not really be at risk for developing psychosis."
Unlike patients in other fields of medicine, those designated mentally ill–or even being declared "at risk" of mental illness lose their autonomy.
Hundreds of thousands of teenagers and young adults (especially those on Medicaid) would be coerced into consuming atypical antipsychotic drugs–even as there is no proof that these expensive drugs prevent psychotic episodes, and despite abundant evidence that these drugs trigger life-long debilitating disease, such as, diabetes and cardio metabolic diseases [3] –and are associated with reduced life expectancy [4]―to say nothing about their high cost, other side effects, and stigma.
Dr. Frances warns that APA’s effort to expand its reach by pathologizing those it deems "at risk" "could lead to a public health catastrophe and no field trial could possibly justify its inclusion as an official diagnosis. The attempt at early identification and treatment of at risk individuals is well meaning, but dangerously premature. We must wait until there is a specific diagnostic test and a safe treatment."
If adopted, the DSM-V Task Force recommendations will vastly INFLATE the patient roster by deeming that healthy people are in need of early intervention for presumed "risk" for illness.
APA’s move occurs just as an avalanche of evidence has exposed psychiatry’s misdiagnosing practices and its failed pharmacological treatments–including the misdiagnosing of American children as "bipolar" for which they were prescribed antipsychotics, the most toxic drugs in pharmacopoeia, whose cost has depleted public healthcare budgets. Psychiatry is attempting to expand its reach by designating healthy people as being "AT RISK" for mental illness IN THE FUTURE–thereby providing a rationale for increased use of psychotropic drugs to the delight of its corporate retainers, the drug manufacturers.
It is clear that the beneficiaries of APA’s expansionist DSM-V revisions are those with vested financial stakes in maintaining high volume sales of clinically dubious, but highly profitable drugs.
References:
1. DSM5 and "Psychosis Risk Syndrome:" Not Ready For Prime Time By Allen Frances, MD, Psychiatric Times, March 19, 2010
2. Opening Pandora’s Box: The 19 Worst Suggestions For DSM5 Commentary By Allen Frances, MD, Psychiatric Times. COMMENTARY, February 11, 2010
3. Cardiometabolic Risk of Second-Generation Antipsychotic Medications During First-Time Use in Children and Adolescents By Christoph U. Correll, MD; Peter Manu, MD; Vladimir Olshanskiy, MD; Barbara Napolitano, MA; John M. Kane, MD; Anil K. Malhotra, MD, JAMA. 2009;302(16):1765-1773
4. A Systematic Review of Mortality in Schizophrenia: Is the Differential Mortality Gap Worsening Over Time? By Sukanta Saha, MSc, MCN; David Chant, PhD; John McGrath, MD, PhD, FRANZCP, Arch Gen Psychiatry. 2007;64(10):1123-1131.
Vera Hassner Sharav
THE NEW YORK TIMES
April 6, 2010
In Medicine, the Power of No
By DAVID LEONHARDT
How can we learn to say no?The federal government is now starting to build the institutions that will try to reduce the soaring growth of health care costs. There will be a group to compare the effectiveness of different treatments, a so-called Medicare innovation center and a Medicare oversight board that can set payment rates.
But all these groups will face the same basic problem. Deep down, Americans tend to believe that more care is better care. We recoil from efforts to restrict care.
Managed care became loathed in the 1990s. The recent recommendation to reduce breast cancer screening set off a firestorm. On a personal level, anyone who has made a decision about his or her own care knows the nagging worry that comes from not choosing the most aggressive treatment.
This try-anything-and-everything instinct is ingrained in our culture, and it has some big benefits. But it also has big downsides, including the side effects and risks that come with unnecessary treatment. Consider that a recent study found that 15,000 people were projected to die eventually from the radiation they received from CT scans given in just a single year — and that there was “significant overuse” of such scans.
From an economic perspective, health reform will fail if we can’t sometimes push back against the try-anything instinct. The new agencies will be hounded by accusations of rationing, and Medicare’s long-term budget deficit will grow.
So figuring out how we can say no may be the single toughest and most important task facing the people who will be in charge of carrying out reform. “Being able to say no,” Dr. Alan Garber of Stanford says, “is the heart of the issue.”
It’s easy to come up with arguments for why we need to do so. Above all, we don’t have a choice. Giving hospitals and drug makers a blank check will bankrupt Medicare. Slowing the cost growth, on the other hand, will free up resources for other uses, like education. Lower costs will also lift workers’ take-home pay.
But I suspect that these arguments won’t be persuasive. They have the faint ring of an insurer’s rationale for denying a claim. Compared with an anecdote about a cancer patient looking for hope, the economic arguments are soulless.
The better bet for the new reformers — starting with Donald Berwick, the physician who will run Medicare — is to channel American culture, not fight it. We want the best possible care, no matter what. Yet we often do not get it because the current system tends to deliver more care even when it means worse care.
It’s not just CT scans. Caesarean births have become more common, with little benefit to babies and significant burden to mothers. Men who would never have died from prostate cancer have been treated for it and left incontinent or impotent. Cardiac stenting and bypasses, with all their side effects, have become popular partly because people believe they reduce heart attacks. For many patients, the evidence suggests, that’s not true.
Advocates for less intensive medicine have been too timid about all this. They often come across as bean counters, while the try-anything crowd occupies the moral high ground. The reality, though, is that unnecessary care causes a lot of pain and even death. Dr. Berwick, who made his reputation campaigning against medical errors, is a promising (if much belated) selection for precisely this reason.
Can we solve the entire problem of rising health costs by getting rid of needless care? Probably not. But the money involved is not trivial, and it’s the obvious place to start.
• Learning to say no more often will be a three-step process, and if the new agencies created by the health act are run well, they can help with all three.
The first is learning more about when treatments work and when they don’t. “All too often,” the Institute of Medicine reports, the data is “incomplete or unavailable.” As a result, more than half of treatments lack clear evidence of effectiveness, the institute found. It says the most promising areas for research include prostate cancer, inflammatory diseases, back pain, hyperactivity, and CT scans vs. M.R.I.’s for cancer diagnosis.
As part of the health act, a Patient Centered Health Research group will have an annual budget of $600 million. Relative to total health spending, that’s a paltry sum. But it’s real money relative to what’s now being spent on such research.
The second step — and maybe the most underappreciated one — is to give patients the available facts about treatments. Amazingly, this often does not happen. “People are pretty woefully undereducated about fateful medical decisions,” says Dr. Michael Barry of the Massachusetts General Hospital, an advocate for sharing more with patients.
Dale Collins Vidal, a reconstructive breast surgeon at the Dartmouth-Hitchcock Medical Center, told me a story about a patient’s husband who asked to sit in on the medical team’s discussion of his wife’s case. The doctors said no, because they were uncomfortable with him knowing about the uncertainty surrounding the case. “The paternalism is a little more kind-hearted than it was in the past,” Dr. Vidal says, “but it’s still paternalism.”
When patients are given information about potential benefits and risks, they seem to choose less invasive care, on average, than doctors do, according to early studies. Some people, of course, decide that aggressive care is right for them — like the cancer patient (and palliative care doctor) profiled in this newspaper a few days ago. They are willing to accept the risks and side effects that come with treatment. Many people, however, go the other way once they understand the trade-offs.
They decide the risk of incontinence and impotence isn’t worth the marginal chance of preventing prostate cancer. Or they choose cardiac drugs and lifestyle changes over stenting. Or they opt to skip the prenatal test to determine if their baby has Down syndrome. Or, in the toughest situation of all, they decide to leave an intensive care unit and enter a hospice.
The health act requires Medicare and other agencies to help hospitals and doctors give patients more information — which is practically a no-lose proposition. In the course of receiving more control and more choice, two distinctly American values, patients will probably help hold down costs.
The final step is the bluntest. It involves changing the economics of medicine, to reward better care rather than simply more care. Health reform doesn’t go nearly far enough on this score, but it is a start.
The tax subsidies for health insurance will shrink, which should help people realize medical care is not free. And doctors who provide good, less expensive care won’t be financially punished as often as they now are.
None of these steps will allow us to avoid the wrenching debates that are an inevitable part of health policy. Eventually, we may well have to decide against paying for expensive treatments with only modest benefits. But given how difficult that would be for this country, it makes sense to start with the easier situations — the ones in which “no” really is the best answer for patients.
“In the United States, I don’t know that we’re ever going to get to a point where we limit health care spending,” as Dr. Vidal says. “But maybe we could get patients to the same place on their own.”
E-mail: leonhardt@nytimes.com