Lawsuits, Just the Cost of Criminal Marketing of Antipsychotic Drugs
A New York Times report (below) reviews what has been accomplished by multiple civil and criminal lawsuits against Big Pharma companies that have relied almost entirely on fraud to market industry’s worst pharmaceuticals–antipsychotic drugs–which have become industry’s most profitable cash cow.
"The new generation of antipsychotics has also become the single biggest target of the False Claims Act, a federal law once largely aimed at fraud among military contractors. Every major company selling the drugs — Bristol-Myers Squibb, Eli Lilly, Pfizer, AstraZeneca and Johnson & Johnson — has either settled recent government cases for hundreds of millions of dollars or is currently under investigation for possible health care fraud."
"Two of the settlements, involving charges of illegal marketing, set records last year for the largest criminal fines ever imposed on corporations. One involved Eli Lilly’s antipsychotic, Zyprexa; the other involved a guilty plea for Pfizer’s marketing of a pain pill, Bextra. In the Bextra case, the government also charged Pfizer with illegally marketing another antipsychotic, Geodon; Pfizer settled that part of the claim for $301 million, without admitting any wrongdoing."
But these lawsuits are no deterrent to crime, as Jerome Avorn, MD, Harvard medical professor correctly observes : "When you’re selling $1 billion a year or more of a drug, it’s very tempting for a company to just ignore the traffic ticket and keep speeding.”
The Times cites several psychiatrists who now validate what critics have been pointing out: the clinical value of antipsychotics is entirely "unclear" "greatly exxagerated" "completely ineffective"
How is it, one must ask, that industry’s paid academic psychiatrists, who are referred to as "key opinion leaders" failed to see for two decades, the elephant before them?
Dr. Jeffrey Lieberman, chairman of psychiatry at Columbia University, who not only vigorously denied the drugs’ adverse effects, he excoriated Robert Whitaker, author of Mad in America, for writing what the scientific evidence shows, now Dr. Lieberman grudgingly acknowledges that the clinical value of antipsychotics–even for the treatment of schizophrenia (for which they were approved) was "greatly exaggerated".
How credible are proclaimed medical "authorities" who claimed to be guided by scientific-evidence, now say they were blinded by industry’s marketing hype into believing the drugs improved patients’ condition?
What professional competence do psychiatrists have if they fail to notice lack of cognitive improvement in their patients, or to fail to notice their patients’ newly developed-de novo–profound medical deterioration and measurable physiological symptoms of chronic disease after beiing on these drugs?
The Times review omits two important players who contributed to the extraordinary marketing success of antipsychotics–drugs whose risks far outweigh any demonstrable benefit.
1. The role of government:
The standard for FDA approval requires evidence of a benefit that outweighs the risks. By that standard, these drugs should never have been approved for use in human beings.
- FDA approval of antipsychotics misbranded antipsychotics as "safe and effective" provided legitimacy to company deception.
- FDA approval for numerous other uses of these dangerous drugs provided a license for ilegitimate use of these drugs, for children, for example.
- In essence, FDA provided a license for market expansion and increase profits–ignoring the mounting evidence against these drugs.
- State and federal governments have actively encouraged the use of these drugs–by adopting industry-formulated prescribing formularies (TMAP );
- providing generous and unrestricted reimbursement even for unapproved multiple drug cocktails through Medicaid, Medicare, Veterans Affairs;
- and government’s role in encouraging coercive measures to force patients to take the drugs that demonstrably harm them.
2. The role of the National Alliance for Mental Illness (NAMI, formerly called National Alliance for the Mentally Ill)
- an industry-paid for front group, 81% of whose income comes from drug manufacturers.
- NAMI betrayed the trust of its constituents–parents of diagnosed people with mental illness–
- Taking their cue from industry-supported psychiatrists who served as promotional reps,
NAMI misled families about the severe, irreversible harm produced by antipsychotic drugs–
failing to inform them about the lack of evidence for their clinical value.
Vera Hassner Sharav
THE NEW YORK TIMES
October 2, 2010
Side Effects May Include Lawsuits
By DUFF WILSON
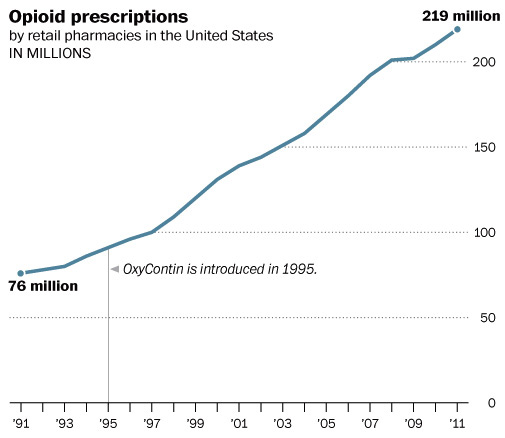
FOR decades, antipsychotic drugs were a niche product. Today, they’re the top-selling class of pharmaceuticals in America, generating annual revenue of about $14.6 billion and surpassing sales of even blockbusters like heart-protective statins.
While the effectiveness of antipsychotic drugs in some patients remains a matter of great debate, how these drugs became so ubiquitous and profitable is not. Big Pharma got behind them in the 1990s, when they were still seen as treatments for the most serious mental illnesses, like hallucinatory schizophrenia, and recast them for much broader uses, according to previously confidential industry documents that have been produced in a variety of court cases.
Anointed with names like Abilify and Geodon, the drugs were given to a broad swath of patients, from preschoolers to octogenarians. Today, more than a half-million youths take antipsychotic drugs, and fully one-quarter of nursing-home residents have used them. Yet recent government warnings say the drugs may be fatal to some older patients and have unknown effects on children.
The new generation of antipsychotics has also become the single biggest target of the False Claims Act, a federal law once largely aimed at fraud among military contractors. Every major company selling the drugs — Bristol-Myers Squibb, Eli Lilly, Pfizer, AstraZeneca and Johnson & Johnson — has either settled recent government cases for hundreds of millions of dollars or is currently under investigation for possible health care fraud.
Two of the settlements, involving charges of illegal marketing, set records last year for the largest criminal fines ever imposed on corporations. One involved Eli Lilly’s antipsychotic, Zyprexa; the other involved a guilty plea for Pfizer’s marketing of a pain pill, Bextra. In the Bextra case, the government also charged Pfizer with illegally marketing another antipsychotic, Geodon; Pfizer settled that part of the claim for $301 million, without admitting any wrongdoing.
The companies all say their antipsychotics are safe and effective in treating the conditions for which the Food and Drug Administration has approved them — mostly, schizophrenia and bipolar mania — and say they adhere to tight ethical guidelines in sales practices. The drug makers also say that there is a large population of patients who still haven’t taken the drugs but could benefit from them.
AstraZeneca, which markets Seroquel, the top-selling antipsychotic since 2005, says it developed such drugs because they have fewer side effects than older versions.
“It’s a drug that’s been studied in multiple clinical trials in various indications,” says Dr. Howard Hutchinson, AstraZeneca’s chief medical officer. “Getting these patients to be functioning members of society has a tremendous benefit in terms of their overall well-being and how they look at themselves, and to get that benefit, the patients are willing to accept some level of side effects.”
The industry continues to market antipsychotics aggressively, leading analysts to question how drugs approved by the Food and Drug Administration for about 1 percent of the population have become the pharmaceutical industry’s biggest sellers — despite recent crackdowns.
Some say the answer to that question isn’t complicated.
“It’s the money,” says Dr. Jerome L. Avorn, a Harvard medical professor and researcher. “When you’re selling $1 billion a year or more of a drug, it’s very tempting for a company to just ignore the traffic ticket and keep speeding.”
NEUROLEPTIC drugs — now known as antipsychotics — were first developed in the 1950s for use in anesthesia and then as powerful sedatives for patients with schizophrenia and other severe psychotic disorders, who previously might have received surgical lobotomies.
But patients often stopped taking those drugs, like Thorazine and Haldol, because they could cause a range of involuntary body movements, tics and restlessness.
A second generation of drugs, called atypical antipsychotics, was introduced in the ’90s and sold to doctors more broadly, on the basis that they were safer than the old ones — an assertion that regulators and researchers are continuing to review because the newer drugs appear to cause a range of other side effects, even if they cause fewer tics.
Contentions that the new drugs are superior have been “greatly exaggerated,” says Dr. Jeffrey A. Lieberman, chairman of the psychiatry department at Columbia University. Such assertions, he says, “may have been encouraged by an overly expectant community of clinicians and patients eager to believe in the power of new medications.”
“At the same time,” he adds, “the aggressive marketing of these drugs may have contributed to this enhanced perception of their effectiveness in the absence of empirical evidence.”
Others agree. “They sold the story they’re more safe, when they aren’t,” says Robert Whitaker, a journalist who has written two books about psychiatric medicines. “They had to cover up the problems. Right from the start, we got this false story.”
The drug companies say all the possible side effects are fully disclosed to the F.D.A., doctors and patients. Side effects like drowsiness, nausea, weight gain, involuntary body movements and links to diabetes are listed on the label. The companies say they have a generally safe record in treating a difficult disease and are fighting lawsuits in which some patients claim harm.
The cases, both civil and criminal, against many of the world’s largest drug makers have unveiled hundreds of previously confidential documents showing that some company officials were aware they were using questionable tactics when they marketed these powerful, expensive drugs.
Such marketing, according to analysts and court documents, included payments, gifts, meals and trips for doctors, biased studies, ghostwritten medical journal articles, promotional conference appearances, and payments for postgraduate medical education that encourages a pro-drug outlook among doctors. All of these are tools that federal investigators say companies have used to exaggerate benefits, play down risks and promote off-label uses, meaning those the F.D.A. hasn’t approved.
Lawyers suing AstraZeneca say documents they have unearthed show that the company tried to hide the risks of diabetes and weight gain associated with the new drugs. Positive studies were hyped, the documents show; negative ones were filed away.
According to company e-mails unsealed in civil lawsuits, AstraZeneca “buried” — a manager’s term — a 1997 study showing that users of Seroquel, then a new antipsychotic, gained 11 pounds a year, while the company publicized a study that asserted they lost weight. Company e-mail messages also refer to doing a “great smoke-and-mirrors job” on an unfavorable study.
“The larger issue is how do we face the outside world when they begin to criticize us for suppressing data,” John Tumas, then AstraZeneca’s publications manager, wrote in a 1999 e-mail. “We must find a way to diminish the negative findings,” he added. “But, in my opinion, we cannot hide them.”
Tony Jewell, an AstraZeneca spokesman, said last week that the company had turned over all that material to the F.D.A. as part of the approval process and updated its label over the years to show the latest safety information.
Dr. Stefan P. Kruszewski, a Harvard-educated psychiatrist who once worked as a paid speaker for several drug makers, became a government informant and now consults for plaintiffs suing drug companies. Earlier in his career, he spoke at events for Pfizer, GlaxoSmithKline and Johnson & Johnson as an advocate of antipsychotics. He said one company offered him incentives of $1,000 or more every time he talked to an individual doctor about one of its drugs.
“When I started speaking for companies in the late 1980s and early ’90s, I was allowed to say what I thought I should say consistent with the science,” he recalls. “Then it got to the point where I was no longer allowed to do that. I was given slides and told, ‘We’ll give you a thousand dollars if you say this for a half-hour.’ And I said: ‘I can’t say that. It isn’t true.’ ”
Slides for one new antipsychotic drug contended that it had no neurological side effects. “They made it all up,” Dr. Kruszewski said. “It was never true.”
The antipsychotics found an easy route around regulations because of the leeway given to many big drug makers.
While drug companies are prohibited from promoting drugs for conditions for which they have not been proved safe and effective, their paid consultants, researchers and educators may do that for them verbally and in company-sponsored studies.
“They can give a small hint, and people will take the bait,” says Dr. Robert Rosenheck, a professor of psychiatry and public health at the Yale School of Medicine, who has received research support from drug makers and federal agencies. “Psychiatric disorders are vaguely defined enough that you can stretch definitions,” he says. “So many treatments are completely ineffective, people are willing to try anything.”
For their part, doctors are free to prescribe any approved drug for any medical condition they choose, even if the drug hasn’t been approved for that specific treatment. “Because they’re approved, they become an alternative for doctors who can’t think of what else to prescribe,” says Dr. Daniel J. Carlat, an associate professor of psychiatry at Tufts University. “Whether they’re useful or not is unclear.”
Analysts said that given the profits that were to be made, the murkiness of mental disorders, and holes in the regulatory regime, marketing excesses were bound to occur.
“If you have a lot of money on the table and you have clinical uncertainty over mental health conditions, where you don’t have a blood test or objective test for it, you see it’s kind of a combustible mixture,” says Dr. Mark Olfson, a Columbia University psychiatry professor and researcher.
DOCUMENTS produced in recent litigation and in Congressional investigations show that some leading academic doctors have worked closely with corporate benefactors to expand the use of antipsychotics.
The most well-known is Joseph Biederman, a Harvard medical professor and Massachusetts General Hospital researcher. His studies, examining prevalence of bipolar psychological disorders in children, helped expand practice standards, leading to a fortyfold increase in such diagnoses from 1994 to 2003. The increase was reported in a 2007 study by the Archives of General Psychiatry.
Between 2000 and 2007, he also got $1.6 million in speaking and consulting fees — some of them undisclosed to Harvard — from companies including makers of antipsychotic drugs prescribed for some children who might have bipolar disorder, a Senate investigation found in 2008.
Johnson & Johnson gave more than $700,000 to a research center that was headed by Dr. Biederman from 2002 to 2005, records show, and some of its work supported the company’s antipsychotic drug, Risperdal.
Dr. Biederman says that the money did not influence him and that some of his work supported other drugs.
“Dr. Biederman’s research does not promote a particular diagnosis or treatment,” his lawyer, Peter Spivack, wrote in an e-mail on Thursday.
The increase in pediatric bipolar diagnosis, the lawyer said, “cannot be attributed solely to Dr. Biederman’s work.” Treatment was expanded to help children and their families, he said.
Mr. Spivack said Dr. Biederman’s disclosure lapses were minor and inadvertent. A Harvard spokesman said they were still under review.
According to government investigators and plaintiffs’ lawyers, many of the studies of antipsychotics were conceived in marketing departments of pharmaceutical companies, written by ghostwriters and then signed by prominent physicians — giving the illusion that the doctors were undertaking their studies independently.
Such practices continue.
“The content is preplanned,” said one doctor who has worked as an uncredited medical writer for antipsychotic studies. Data is used selectively and interpreted for company benefit, said the doctor, who still works in medical writing and spoke on the condition of anonymity to preserve future job prospects.
“Review articles and original research articles have advertising messages in them,” the doctor said. “That’s part of the plan.”
Such papers influence medicine in many ways, as sales representatives show them to doctors and future research builds upon them.
ACCORDING to the Justice Department, drug companies trained sales reps to rebut valid medical concerns about unproved uses of antipsychotics. For example, the department says, Lilly produced a video called “The Myth of Diabetes” to sell Zyprexa, which became its all-time best-selling drug, even though evidence showed that Zyprexa could cause diabetes, as well as other metabolic problems.
Lilly salespeople also promoted a “5 at 5” drug regimen in nursing homes — 5 milligrams of Zyprexa at 5 p.m. to settle down agitated older patients for the night. A Lilly spokesman declined to say when those sales campaigns occurred. But in 2005, after a new analysis of 15 previous studies, the F.D.A. issued a public health advisory saying the use of antipsychotics to calm older dementia patients would increase risk of death from heart failure or pneumonia. The F.D.A. asked drug makers to add a special warning about that on packaging.
Over the years, as psychiatrists learned more about the drugs’ risks, companies promoted them more to family doctors, pediatricians and geriatricians. Pfizer paid more than 250 child psychiatrists to promote its antipsychotic, Geodon, at a time when it was approved only for adults, according to a government filing with the Pfizer settlement last year.
High-prescribing doctors pocketed extra money in the form of research payments, speaking fees, gifts, meals and junkets — some of which the government has specifically termed illegal “kickbacks.”
In its suit against AstraZeneca, the government produced documents showing that the company paid a Chicago psychiatrist, Dr. Michael Reinstein, nearly $500,000 over a decade to do research, travel and speak for it — even as he led a Medicaid practice he had described to the company as one of “the largest prescribers of Seroquel in the world.”
Dr. Reinstein and AstraZeneca have both denied any misconduct.
In April, AstraZeneca became the fourth major drug company in three years to settle a government investigation with a hefty payment — in its case, $520 million for what federal officials described as an array of illegal promotions of antipsychotics for children, the elderly, veterans and prisoners. Still, the payment amounted to just 2.4 percent of the $21.6 billion AstraZeneca made on Seroquel sales from 1997 to 2009.
LAST year, Eli Lilly and Pfizer settled investigations resulting in the largest criminal fines in United States history. Lilly paid a $515 million criminal fine as part of a broader, $1.4 billion settlement with the government. Pfizer later paid a $1.3 billion criminal fine as part of a broader, $2.3 billion settlement.
The Lilly case focused entirely on its antipsychotic drug Zyprexa, while Pfizer’s settlement included $301 million related to its antipsychotic, Geodon, along with marketing of other drugs.
In 2007, Bristol-Myers Squibb paid $515 million to settle federal and state investigations into marketing of its antipsychotic drug Abilify to child psychiatrists and nursing homes. Bristol-Myers Squibb, like AstraZeneca, denied any misconduct.
Johnson & Johnson is currently under investigation by the Justice Department, which says it paid kickbacks to induce Omnicare, the nation’s largest nursing home pharmacy, to recommend Risperdal, government filings show. Omnicare paid $98 million last November to settle civil charges.
J.& J. is fighting a government lawsuit and says in court filings that it was paying rebates — an argument endorsed in a filing by the industry trade group, the Pharmaceutical Research and Manufacturers of America.
Some officials at companies say they’ve made systemic changes to avoid illegal marketing of antipsychotics and other products.
“That was a blemish for us,” John C. Lechleiter, Eli Lilly’s chief executive, said in an interview. “We don’t ever want that to happen again. We put measures in place to assure that not only do we have the right intentions in integrity and compliance, but we have systems in place to support that.”
Jeffrey B. Kindler, Pfizer’s chief executive, voiced similar thoughts in an interview. “Never again,” he said. “I take this very seriously.”
Mr. Kindler is operating under Pfizer’s third corporate accountability agreement, a five-year promise to the federal government to reform sales behavior, monitor employees and disclose misconduct. The first was signed in 2002 for withholding rebates for Lipitor. The second, in 2004, was for illegal marketing of the seizure drug Neurontin. The third, last year, was for illegal marketing of the painkiller Bextra.
Pfizer officials say they inherited the first two situations with their acquisitions of two other companies, Warner-Lambert and Parke-Davis.
“It wasn’t our people,” says Douglas Lankler, a senior vice president and chief compliance officer at Pfizer.
Lew Morris, chief counsel for the inspector general of the Department of Health and Human Services, says he is serious about bolstering government efforts to reform or punish drug makers for illegal sales of antipsychotics.
“The message we want to send to the industry is it’s not just the same-old, same-old,” he said in an interview.
He agrees that few industry employees have gone to jail for white-collar crimes, but says this may change soon. “We’re targeting managers and executives who should have known,” he said.
Mr. Morris says some companies are “too big to debar” from government contracts, since doing so would just hurt patients needing medicine. But he says discussions are under way about forcing one health care company to sell off a subsidiary accused of fraud. And directors who ignore information may face more risk of shareholder suits, he says.
Over the next year, the government is adding at least 15 prosecutors and 100 investigators to pursue health care fraud.
The Pharmaceutical Research and Manufacturers of America, also strengthened its marketing code of conduct two years ago, banning gifts and meals, although salespeople can still bring meals to doctors’ offices.
Some companies are also disclosing their consulting and speaking payments, as required by the government agreements. And groups in charge of medical writing and postgraduate education have taken steps to disclose or reduce industry influence.
But more than 1,000 False Claims Act lawsuits are still under way, most of them focused on health care and many on lucrative antipsychotic drugs. For that reason alone, critics say they think the industry still hasn’t gone far enough to change questionable practices.
“The drug industry still rewards sales,” says Stephen A. Sheller, a lawyer who has represented whistle-blowers in the Lilly and AstraZeneca cases. “And it’s still easy to market these drugs to doctors who are rushed.”